Categories
Change Password!
Reset Password!

To determine the rate of alteration in longitudinal cervical length after randomly assigning females having a record of failed vaginal cerclage to receive one of three cerclages: low transvaginal, high transvaginal, or transabdominal.
Cervical length measurements are useful predictors of spontaneous preterm birth in women, with preconception transabdominal cerclage offering greater advantages in preserving cervical integrity at the level of the internal os.
To determine the rate of alteration in longitudinal cervical length after randomly assigning females having a record of failed vaginal cerclage to receive one of three cerclages: low transvaginal, high transvaginal, or transabdominal.
The study analyzed longitudinal transvaginal ultrasound measurements of cervical length from the participating women. This trial involved a randomized controlled comparison of transabdominal cerclage (TAC), high transvaginal cerclage, and low transvaginal cerclage. The cervical length estimations at particular gestational ages over time and between the different cerclage groups were compared using statistical analysis methods.
A comparison of cervical length measurements in women who had TAC placed before pregnancy versus during pregnancy was also done. The study also investigated about using cervical length as a diagnostic predictor of spontaneous preterm birth before 32 weeks of pregnancy.
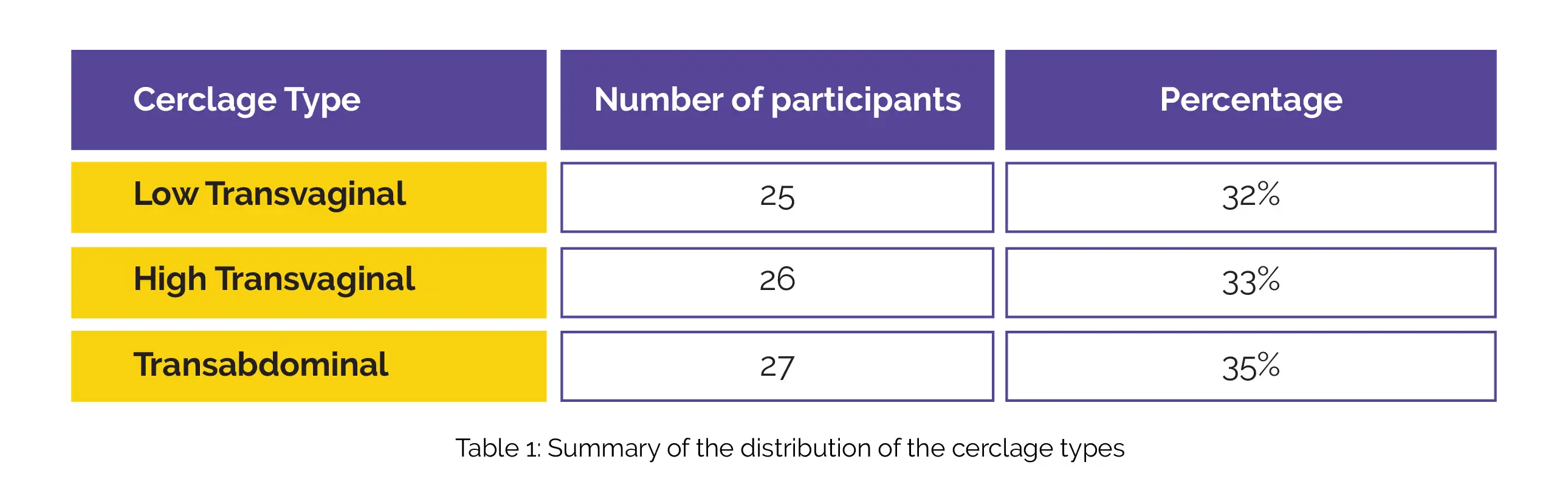
Seventy-eight women with a history of failed cerclage who underwent longitudinal cervical length assessment (details below) were included in this study, Table 1:
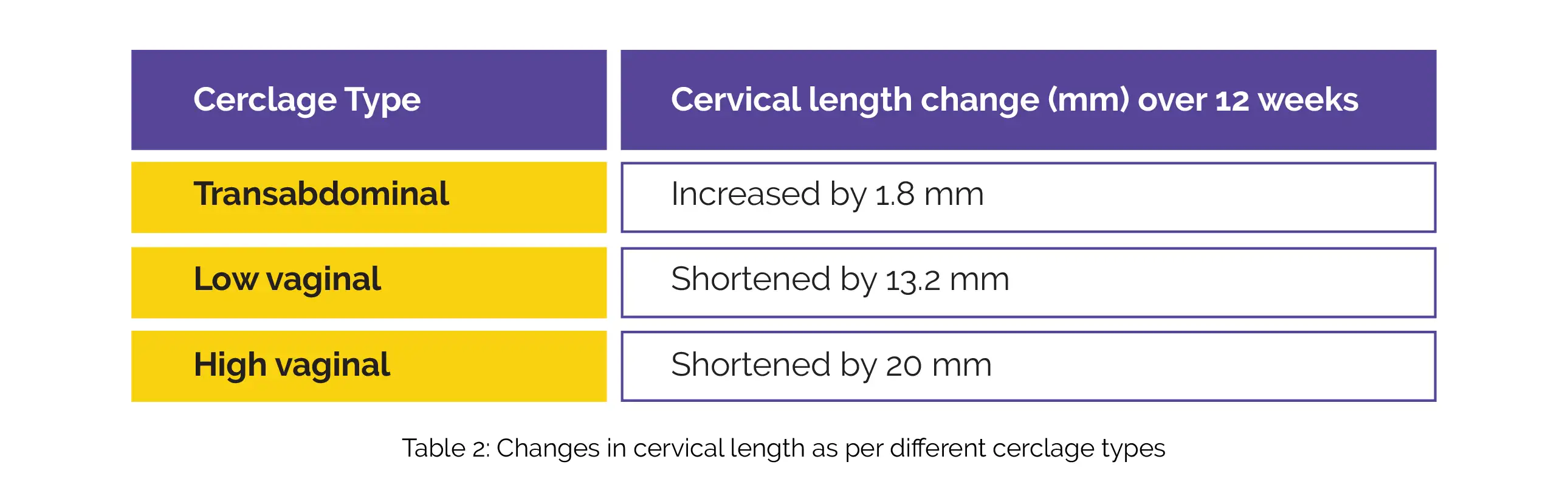
During the surveillance period of 14 to 26 weeks of gestation, abdominal cerclage demonstrated superiority in maintaining cervical length compared to both low and high vaginal cerclage. The difference in cervical length change was +0.08 mm/week, with a 95% confidence interval of -0.40 to 0.22. Over the 12-week surveillance period, women who underwent TAC experienced an average increase of 1.8 mm in cervical length (+1.8 mm; 95% confidence interval, −7.89 to 4.30).
In terms of preventing cervical shortening, high vaginal cerclage showed no significant advantage over low cervical cerclage. Among those with low vaginal cerclage, the cervix shortened by 13.2 mm over 12 weeks (95% confidence interval, −21.7 to −4.7), while for those with high vaginal cerclage, the cervix shortened by 20 mm over 12 weeks (95% confidence interval, −33.1 to −7.4), as shown in Table 2:
TAC performed before conception led to a greater cervical length compared to procedures performed during pregnancy. The significant difference between the two groups became evident after 22 weeks of gestation (48.5 mm vs. 39.6 mm). Furthermore, cervical length proved to be an outstanding predictor of spontaneous preterm birth at less than 32 weeks of gestation, with an excellent receiver operating characteristic curve of 0.92 (95% confidence interval, 0.82-1.00).
In women who have experienced a failed vaginal cerclage, the cervical length tends to funnel and shorten over time in subsequent pregnancies when treated with vaginal cerclage. In contrast, TAC helps maintain cervical length, and preconception procedures are more effective in preserving the cervix's structural integrity.
American Journal of Obstetrics and Gynecology
Longitudinal change in cervical length following vaginal or abdominal cervical cerclage: a randomized comparison
Alexandra E. Ridout et al.
Comments (0)